A deeper look into the private insurance gap driving America’s rural health crisis
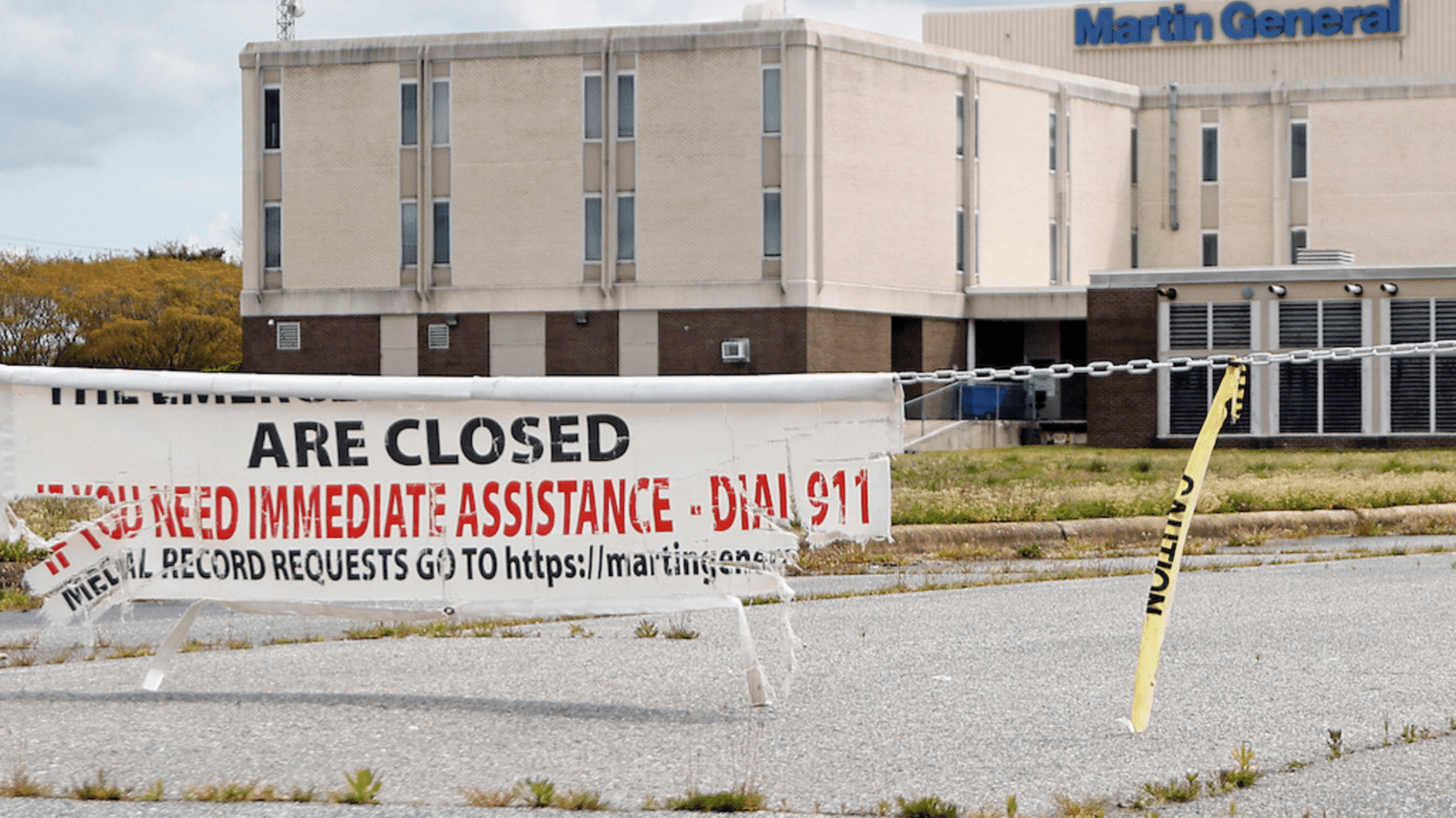
The closure of rural hospitals across the United States has reached alarming levels, with over 100 rural hospitals shutting down in the past decade. While many assume this crisis stems from issues with Medicaid reimbursements, new insights reveal a less obvious but more damaging culprit: private insurance.
According to a detailed investigation by Time, rural hospitals often get paid far less by private insurers than their urban counterparts—despite similar or even higher operational costs. This imbalance is widening the financial gap, pushing rural medical centers toward insolvency.
Image credit: Karl B Deblaker
The Private Insurance Reimbursement Gap
- Urban hospitals tend to have stronger negotiating power due to larger patient volumes and greater access to provider networks.
- Rural hospitals, serving smaller, often poorer populations, accept lower private insurance reimbursements—sometimes just a fraction of the rates paid to urban facilities.
- While Medicare and Medicaid generally pay uniform rates nationwide, private insurers set their own prices, often squeezing under-resourced rural facilities.
“It’s not Medicaid that’s failing us—it’s the market dynamics of private insurance,” said Harold Miller, president of the Center for Healthcare Quality and Payment Reform.
Consequences for Rural Communities
- Residents lose lifesaving emergency care access, with some needing to travel over 40 miles to reach the nearest emergency room.
- Rural closures also disrupt maternal health services, primary care, and chronic disease management.
- Job loss in healthcare sectors worsens local economies already struggling with low population growth.
Legislative and Policy Efforts
Several lawmakers are now calling for federal intervention, proposing initiatives like the Rural Hospital Stabilization Act and payment parity reforms that would enforce fairer reimbursement standards for rural facilities.
Meanwhile, rural health leaders are urging the Centers for Medicare & Medicaid Services (CMS) to pressure insurers into more transparent and equitable pricing.
Why This Matters
With nearly 1 in 5 Americans living in rural areas, the loss of these hospitals is not just a medical issue—it’s a public health emergency. Preserving rural healthcare infrastructure is vital for emergency preparedness, maternal health, chronic care, and economic stability in underserved regions.
Source: Time Magazine – The Surprising Reason Rural Hospitals Are Closing